During Thailand’s rainy season, a significant surge in COVID-19 cases has affected infants and school-aged children, particularly after schools reopened for in-person learning. Classrooms with high-density interactions and the spread of more transmissible variants have heightened infection risks. Pediatric cases now account for a notable percentage of daily infections, stressing healthcare capacities and prompting expanded pediatric care facilities. Increased surveillance, targeted vaccination, and strict on-campus measures are being enforced to protect children. Further details reveal broader impacts on families and education.
Although the COVID-19 pandemic has affected populations worldwide, recent surges in Thailand have particularly impacted the country’s youngest demographic, including children and infants. As schools across Thailand reopened during the rainy season, the risk of increased exposure and virus transmission among students became more pronounced. The reopening of educational institutions and the resumption of in-person activities led to higher rates of close contact among children, elevating transmission risks and contributing to a noticeable spike in pediatric cases. The spread of the Delta variant in June 2021 resulted in the country recording over 20,000 new infections daily at its peak.
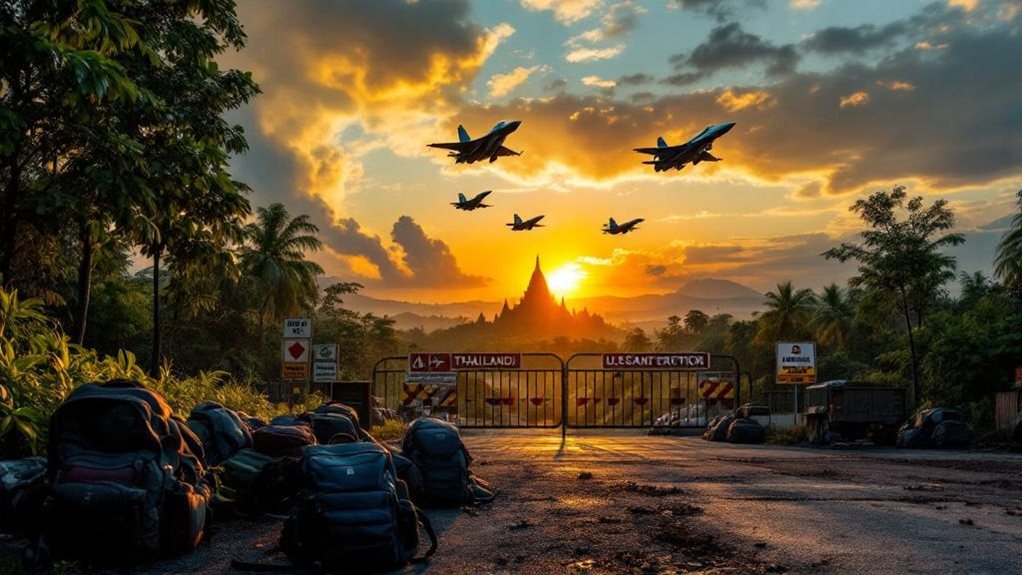
Thailand’s youngest face heightened COVID-19 risks as school reopenings and the Delta variant drive a surge in pediatric cases.
Children under the age of 18 have consistently made up less than 15% of total confirmed cases, but the vulnerability of this group remains a significant concern. Young children, particularly those with incomplete vaccination series or underdeveloped immune systems, have faced greater risks of severe outcomes. During the Delta outbreak, the mortality rate among pediatric cases in Thailand was approximately 0.83%. Following the end of national surveillance measures, excess mortality among children in Thailand increased, especially among those aged 2 to 3 years. Reporting delays impact daily case figures and can make it challenging to assess the real-time burden of COVID-19 among Thailand’s youngest.
Transmission peaks coincided with the timing of school reopenings and public holidays, highlighting the close relationship between social behavior and infection trends. Healthcare systems responded by expanding pediatric care facilities, introducing field hospitals, and implementing home isolation options to manage capacity. Resources were reallocated to prioritize severe cases, and a zoning system was used to classify patients according to symptom severity, which improved triage and treatment efficiency.
Vaccination campaigns targeting eligible children and educational staff were accelerated, and strict public health measures, such as social distancing and mask mandates, were enforced within schools. Socio-economic disparities further complicated the impact of the surge. Families experiencing economic hardship faced challenges accessing healthcare and maintaining adequate nutrition for children.
Mitigation measures like school closures and social distancing, while necessary for infection control, also had social and educational repercussions for younger populations. Continued surveillance, reporting, and targeted vaccination policies remain essential in managing transmission and protecting Thailand’s youngest citizens as the pandemic evolves.